When the COVID-19 pandemic began, it wasn’t hard to predict that incarcerated people would be at higher risk. Many prisons and jails are crowded, dirty places with inconsistent access to health care: a breeding ground for the highly infectious virus. But we’re still waiting for an official count of how many more people died because they were behind bars, and the job of documenting the deaths has fallen to a patchwork of research groups and reporters.
Now, a new national study out of one of these collaborations between the University of California, Irvine and Brigham and Women’s Hospital shows that at the peak of the pandemic in 2020, people inside prisons died almost three and a half times more frequently than the free population.
Over 6,000 incarcerated people died in the first year of the pandemic, researchers found, using numbers they collected from state prison systems and the Federal Bureau of Prisons. A Marshall Project analysis of data the researchers released shows the overall prison mortality rate spiked at least 50%, and potentially exceeded 75%, with roughly 50 or more people dying per 10,000 in prison in 2020.
The virus hit older generations especially hard, the study’s data shows. Not all states shared counts by age. But in the eight states that did, death rates for people aged 50 and older rose far higher than for others, “reaffirming how much more vulnerable older prisoners are,” said the study’s lead author, Naomi Sugie.
Death rates for older incarcerated people spiked in 2020
These death rates are approximated using the number of deaths for every 10,000 people in custody at the start of the year. The 2020 spikes shown probably underestimate the true rise in death rates, since many prison populations fell as the year went on.
Aged 65 or older
In 2020, at least 150 more people in prisons died per 10,000 compared to 2019
Aged 50 to 64
Almost 30 more deaths
Aged 49 or under
About 1 more death
Source: Marshall Project analysis of data published by the University of California, Irvine and Brigham and Women’s Hospital.
At the same time, incarceration rates dropped during the first year of the pandemic, but not because an extraordinary number of people were released. Despite a range of advocates calling for releases — particularly for older adults, who have higher health risks and statistically lower chances of committing a crime — data shows fewer people than in a typical year were let out in 2020. Instead, there was a dramatic reduction in prison admissions.
The slowdown in admissions meant that prison systems reduced the number of younger people exposed to COVID, while the older people already inside were left there. That’s because incarcerated people are generally older than those likely to be sent to prison.
By the end of 2020, Bureau of Justice Statistics data shows the number of people in state prisons under 55 fell by 17%, while the 55 and older population was down by 6%.
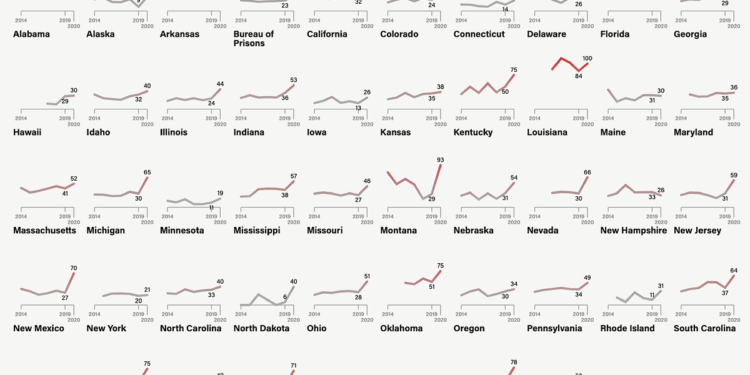
Prison deaths spiked almost everywhere across the country, varying in magnitude from state to state.
Most states had large increases in prison death rates in 2020
These death rates are approximated using the number of deaths for every 10,000 people in custody at the start of the year. The spikes in 2020 probably underestimate the true rise in death rates, since many prison populations fell as the year went on.
Source: Marshall Project analysis of data published by the University of California, Irvine and Brigham and Women’s Hospital.
States and the federal government have legal tools to release at least some people, but rarely used them during the most urgent phase of the pandemic.
In most states, only the governor and parole board can release people from prison without a court order.
Most state constitutions allow for governors to issue a pause in a criminal sentence known as a reprieve. Historically, governors use this power even less often than commutations, which lets them shorten sentences and free people without post-release supervision or expectation that they return. No state governors used either power for large-scale releases during the COVID-19 emergency, and only a small number performed any at all.
Rachel Barkow, a law professor at New York University, called the lack of action a “naked political calculation,” tied to concerns that even a single high-profile crime by someone who was released could turn into a media firestorm. “They didn’t want to take a political risk to do the right thing,” Barkow said of the governors.
Most people let out from state prisons due to COVID-19 were released by parole boards. In Iowa, the parole board held more hearings and released slightly more people in 2020 than in 2019. The state’s Department of Corrections said that administrative changes intended to reduce population numbers in 2020 allowed them to assess parole cases at a higher volume.
Department spokesperson Zach Carlyle said that in the years that followed, the rate at which people who were released committed new crimes went down. “The data showed that despite a higher volume of releases during the pandemic, public safety had not been compromised,” Carlyle said.
But Iowa was an outlier when it came to releases. Parole boards vary widely from state to state, in their composition and how laws and political pressure play on their decisions, and most states released fewer people in 2020 than in previous years. Some officials cited the technical challenges of holding hearings and board meetings during lockdowns and social distancing efforts, while others said any reduction was simply due to normal fluctuations in the number of people eligible for parole in a given year. In other cases, people were approved for parole, but found themselves stuck in prison because the pandemic delayed the required reentry courses. “Truth-in-sentencing” laws — which prevent parole boards from releasing anyone before they’ve served most or all of a minimum sentence — were another key roadblock.
In a minority of states, corrections officials have some limited authority to release prisoners — usually due to terminal illness, or total physical or cognitive disability — or to seek certain kinds of inpatient medical care, according to data collected by the sentencing reform advocacy group Families Against Mandatory Minimums. These policies are not designed to release people based on risk of future illness, however. One exception was Minnesota, where the state granted 158 medical releases after temporarily expanding its program to those at risk for “bad outcomes” from the disease.
In addition to releases, prison systems used various mitigation efforts to slow the virus. Prison officials in Vermont, as well as prisoner advocates at the ACLU of Vermont, said the state took swift action to stop the spread of the disease with aggressive testing and by locking down their facilities. Vermont was the only state that reported zero COVID deaths in its prisons.
But the agency is still dealing with the fallout of keeping people in their cells for such long stretches, said Vermont Department of Corrections Commissioner Nick Deml. “When you’re in lockdown for months on end, that has a huge physical, mental, and emotional toll on human beings,” Deml said. “Imagine being in a room with fluorescent lights, maybe you have some windows here and there, but you’re inside for a year straight.”
Advocates say that other states’ mitigation efforts were less aggressive. Alan Mills, executive director of Uptown People’s Law Center, an organization that supports the rights of incarcerated people in Illinois, said the state didn’t act fast enough to implement such protections. Mills said speed is essential with infectious disease, and that most deaths happened early on, but the state prison health care system was already threadbare and unprepared to handle the pandemic. Illinois had to call in the National Guard to provide basic support, like taking people’s temperatures, as deaths climbed.
The state’s medical system is still struggling, according to a recent report by an independent expert hired by the federal courts. The monitor noted improvements in infection control, but said the system has yet to “establish the foundations of an adequate medical program.”
In 2021, Illinois passed the Joe Coleman Act, which allows the release of sick and older people. The law was celebrated as a tool that would relieve stress on the decrepit prison health care system. But far fewer people have been released than expected. An analysis from Injustice Watch and WBEZ found the state denied nearly two-thirds of medical release requests from people who met the act’s medical criteria.
Naomi Puzzello, spokesperson for the Illinois Department of Corrections, said it’s often difficult to find nursing homes that will take older incarcerated people, so they remain in prison.
Commissioner Deml said Vermont faces the same hurdle. “There are 20, maybe 30 individuals in our prison system today that, if I had a nursing facility that would accept them, I would put them in that facility. They don’t need the security levels that we have.”
While the data collected by the universities sheds new light on the toll of the virus, the federal government still has not publicly released official statistics. That’s because the Bureau of Justice Statistics stopped collecting data on deaths in correctional facilities in 2019, transferring the job to the Bureau of Justice Assistance, another branch of the Department of Justice. The agency has not announced plans on when or if they will publish mortality data again.
The legislative change coincided with the start of COVID’s spread across the U.S., an especially crucial moment to track deaths. “This is a time period we really needed to know the impact of COVID,” said lead researcher Sugie. Instead, groups like Sugie’s spent years collecting the data themselves.
“This is really both to have an accounting of what happened,” she said, “but also, really importantly, to learn from what happened, so we don’t do this again in the future when we have another pandemic, another crisis.”